Product Overview
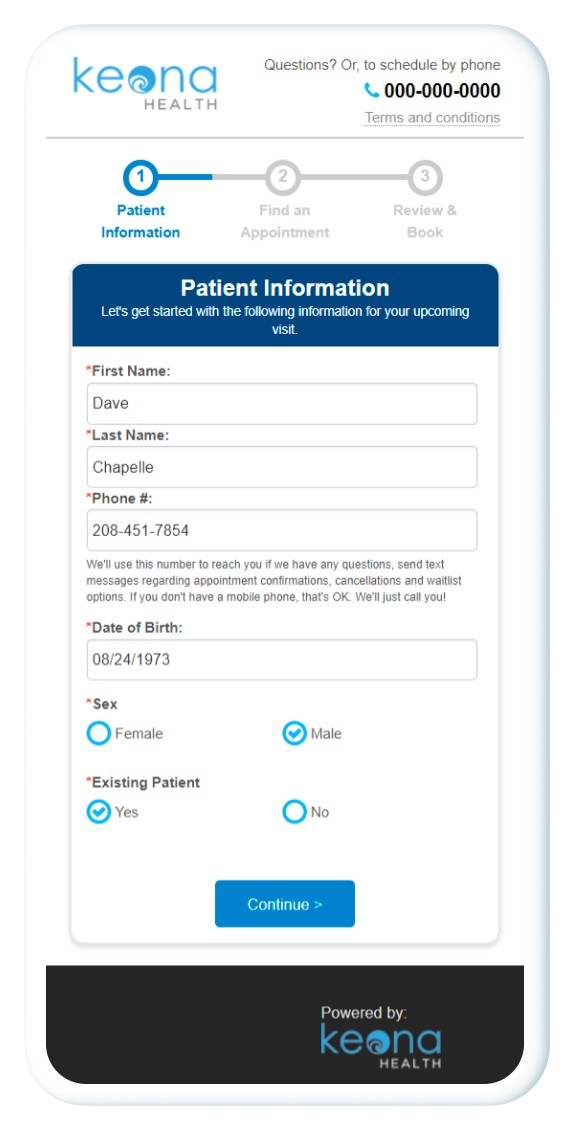
Patient Self-Scheduling
Designed For Providers , Made For Patients
FOR CALL HANDLERS AND NURSES:
Equip your call agents and clinical staff with protocols to guide them through the call handling process. Take advantage of gold standard Schmitt Thompson protocols and/or create your own to accommodate your needs. Tight integration with your EMR presents your staff with all relevant patient information on a single screen, allowing them to make more informed decisions.
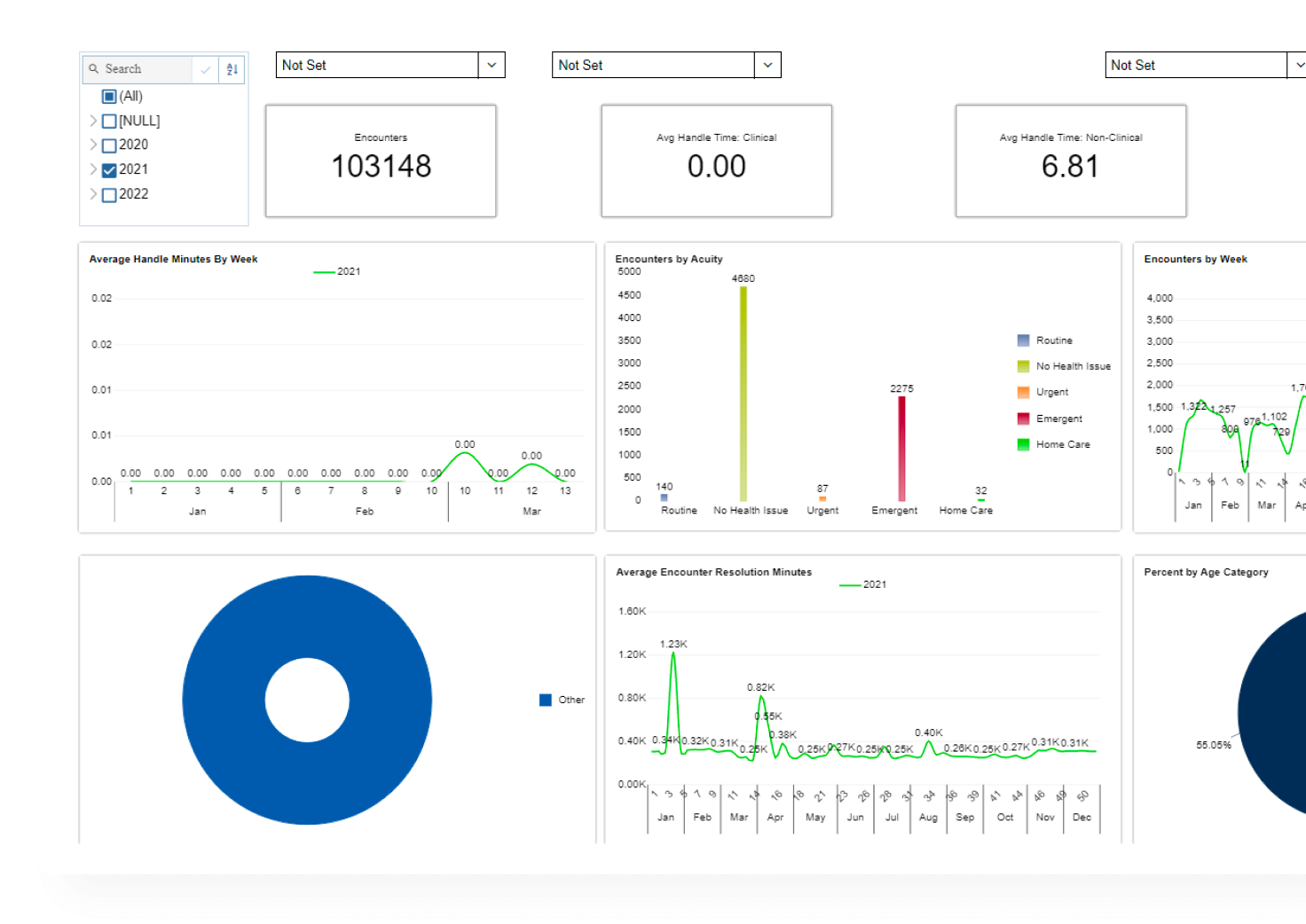
FOR ADMINISTRATORS AND MANAGERS:
Empower your managers with Health Desk’s advanced reporting and analytics suite. Monitor and improve important call center metrics such as first call resolution rates and call handling time.
FOR PATIENTS:
Increase patient access and reduce call volume by offering E-visits. Improve patient satisfaction by ensuring that all calls are properly handled and returned in a timely manner.
Specifications
Patient Scheduling
(Care)fully Designed for Providers
Provider Preferences Encoded
Equitable Distribution of Appointments
Campaigns with Scheduling, Rescheduling & Cancellation
100% Accuracy.
How does Keona’s Patient Self-Scheduling work?
Our highly optimized healthcare scheduling software gives both patients and providers exactly what they need 24/7, anywhere
Download our Patient Self-Scheduling Whitepaper
Keona’s AI-powered medical appointment scheduling software automates complex schedules without sacrificing provider control.
Telephone Nurse Triage: Best Practices For Stellar Telehealth Nursing
What does a telephone triage nurse do?
Telephone triage, also known as telehealth nursing, has existed since the 1960s—but it has never been more important, relevant, and respected than it is today. And for good reason: telephone triage and virtual triage are vital components of modern and holistic healthcare services, much of which are now delivered remotely.
Telephone triage nursing shares many similarities with in-person triage nursing—although there are key differences. Telephone triage nurses are specially trained, registered nurses who work for healthcare providers remotely. Telephone triage nurses work at a variety of locations: healthcare call centers, urgent care centers, emergency departments, and other medical facilities.
To become a telephone triage nurse, attending nursing school or an accredited nursing program is required. Telephone triage nurses are expected to deliver the same quality of care as nurses who work in-person at emergency rooms or physicians' offices.
Telephone triage nurses give care and consultation, over the phone and online, to patients seeking medical treatment. A telephone triage nurse, through a series of questions, assesses the patient's condition, then directs the patient to appropriate medical services.
The telephone triage nurse is responsible for evaluating the patient's symptoms—fever, abdominal pain, cough, chest pain, etc.—then making an appropriate and safe care recommendation. Telephone triage nurses, like in-person registered nurses, must adhere to established guidelines, protocols, and procedures: escalation, duty to terrify, therapeutic rapport, etc.
A telephone triage nurse must accurately assess the patient's condition as quickly as possible, without actually smelling, seeing, and touching the patient—which requires a specific set of skills. Not all registered nurses are fit to become a telephone triage nurse.
Why telephone triage nursing is extremely important for healthcare providers
Many patients now seek medical services remotely. It's called telehealth, and it has become enormously popular in the last few years.
Telephone triage nurses therefore have one of America's most essential professions. They are the key cog in the telehealth machine.
As such, it is vital that telephone triage nurses are properly trained—because the health of millions of people depends on it.
For telehealth nurses, achieving the golden trifecta of safety, efficiency, and care quality is made much easier with the help of healthcare CRM software, which centralizes all patient and provider data into a single platform, so that it is automatically available to the telephone triage nurse whenever a patient calls.
Without healthcare CRM software, telephone triage nurses must navigate a labyrinth of disparate systems, electronic medical records, and apps—which cripples efficiency, care quality, and patient satisfaction.
The telephone triage nursing process
During their consultations with patients, telephone triage nurses evaluate the patient's symptoms and medical history. The telephone triage nurse then offers treatment advice or directs the patient to healthcare services, including:
A specialist physician's office who treats the patient's specific medical needs.
Emergency medical facilities—if the patient's condition calls for it.
The patient's primary care physician, regular doctor, or other local doctors.
Telehealth services (a remote appointment with a physician).
An alternative medical facility, doctor's office, or urgent care clinic.A telephone triage nurse's patient assessment, if executed effectively, increases the likelihood of a positive patient outcome. An inaccurate or incomplete patient assessment, conversely, can lead to a poor patient outcome.
It is thus imperative that telephone triage nurses are equipped with the skills and credentials needed to successfully perform their jobs and deliver the best possible patient care.
Key telehealth nursing skills & credentials
To ensure every telephone triage nurse hired by your organization will excel in the role, look for these attributes:
A degree from a nursing school or an accredited nursing program.
Stellar verbal and non-verbal communication skills.
Experience answering calls, and a keen ability to communicate effectively with patients over the phone.
Willingness to work nontraditional hours, including night shifts.
Experience working in emergency treatment.
Critical thinking skills, and a talent for accurately assessing a patient's condition quickly.
A deep commitment to delivering quality patient care.
The ability to create, when talking with patients over the phone, a mental image of the patient. This allows the nurse to offer personalized care.
Willingness to work for a typical telephone triage nurse salary: roughly $30/hr.
Telephone triage nurses—all medical professionals, really—need common sense and good instincts. Telephone triage nurses must stay calm and prudent, in a high-pressure environment, so that they can confidently and correctly direct patients to the appropriate level of care. Telephone triage nurses generally take on a higher patient load than do in-person nurses, so exercising keen judgment, in the moments that matter, is essential.
Because telephone triage nurses work over the phone, astute listening skills are imperative, for obvious reasons.
Providers, when building and refining their telephone triage system, must commit to a core set of principles. The following 5 axioms should serve as the foundation of your telephone triage operations:
The 5 Telephone Triage Truths
Telephone nursing is safe & effective.
Telephone triage services are grounded in the Standards of Care, developed by the American Association of Ambulatory Care Nurses (AAACN).
The telephone triage process should be performed by specially trained, registered nurses, who have an average of 5 - 10 years of experience in Emergency Treatment and Primary Care, Medical Surgical Nursing, and Pediatrics.
The telephone triage practice is guided by evidence-based clinical guidelines, which are physician approved and updated annually.
But decision support tools are just that, guidelines, not algorithms. Qualified registered nurses understand that each patient encounter is unique. They have critical thinking skills—which are incredibly important when caring for patients remotely—because observing, smelling, and palpating are not an option. Expertise in astute active listening and therapeutic communication is critical.
Quality assurance monitoring of triage phone calls indicates that, in 97% of encounters, telephone triage nurses recommended patients to the appropriate level of care. This extraordinary number illustrates that telephone triage nurses can be trusted to accurately assess patients.
Telephone triage contributes to optimal patient outcomes.
The Institute for Healthcare Reform (IHI) identifies three core objectives for healthcare in the United States:
Enhance the patient experience and patient care.
Improve the population health of certain groups.
Reduce the per capita cost of healthcare.
Telehealth nursing helps fulfill these goals. Telephone triage nursing is a healthcare service that, for each patient, is done on a 1:1 basis. Because of this, telephone triage nursing is:
Foundational to most primary care practices.
Extremely cost effective.
Consolidates services and information across enterprises.
To lower your expenses, streamline your workflows, and improve your patient care, building and refining a sophisticated telephone triage system, one that optimizes the delivery of telehealth services, is crucial.
Telephone triage nurses' work creates an exceptional patient experience.
Telehealth nursing helps providers achieve their patient engagement goals. An organization committed to exceptional patient experiences is an organization that gives patients 24/7 access to telephone triage services.
Healthcare consumerism trends are transforming the healthcare marketplace. Studies indicate that modern consumers demand seamless digital access to all services—including healthcare services.
In the recent past, to receive acute medical care, patients' only option was to go to the emergency room. But thanks to increasingly sophisticated telehealth software, patients can now access healthcare services anywhere and anytime.
Telephone triage nurses don't just evaluate the patient's health; they also provide a timeline for care. Telephone triage calls often don't result in a trip to the emergency room because patients get the care they need from the telephone nurse. Patients don’t need to drive across town to medical offices, nor wait in a crowded waiting room for hours.
Telephone triage greatly enriches the patient experience—which ultimately means more patient acquisition/retention for healthcare organizations.
Telehealth nursing reaps big financial benefits for healthcare providers.
Executive leadership at healthcare organizations should consider investing in AI-powered triage and call support software. Outsourcing calls to a well-regarded contact center is another option.
ROI valuations for providers who invest in an AI-powered call support system are impressive. Telephone triage operations equipped with AI-powered software are far more efficient and effective than operations that are not. A standard telephone nurse handles 2 calls per hour; an AI-equipped telephone nurse handles 4 calls per hour. At a $30/hr salary, that is an exceptional bargain.
For providers hesitant to invest in triage software, one way to dilute the initial expense is to partner with an outsourcing call center company. Many healthcare organizations have made permanent outsourcing arrangements, reaping all the benefits of a telephone triage system with no capital expenditures. It's important for providers to remember that telephone triage is an investment—not an expense.
AI-powered telehealth nursing is a fantastic solution to the alarming nurse staffing shortages—a crisis that keeps the C-Suite awake at night. Thanks to triage software, 24/7 medical care is available to patients, which lowers their risk of escalating to a higher acuity simply because their provider’s office is closed.
And because AI-powered telephone triage creates an integrated care system, it not only improves outcomes; it also boosts internal referrals.
Telephone triage nurses' work helps medical providers better utilize scarce resources.
This is particularly important for overcrowded emergency medical facilities and overburdened primary care providers. Many trendy readmission prevention programs managed by telephone triage nurses are proving successful. Continuous care improves the bottom line in the current fee-for-value reimbursement system. This is just one example of the positive impact a fully-optimized telephone triage system can have on your organization.
To best serve the medical needs of your patients, and to ensure your organization maintains its competitive edge, your leadership must view telehealth nurses as a necessity, not a luxury.
Telephone triage services are being skillfully and compassionately performed by thousands of registered nurses across the country. There are several different models of telephone triage that can be customized to the needs, strengths, and goals of your organization.
Below I've outlined some training techniques and strategies that providers can utilize to get the most out of their telephone triage operations.
Telephone triage training, techniques, & education
Comprehensive Relevant Training is the responsibility of the organization. It is owed to triage nurses, and it is essential for success. When training and hiring your telephone triage nurses, follow these 13 guidelines:
For every new hire, ingrain this belief: Optimal patient outcomes supersede all benchmarks.
Trainers should make no assumptions. They should train every new hire, even if the new hire has ample in-person nursing experience, as if they were fresh out of nursing school. Telehealth nursing requires a different skill set than in-person nursing—so every new employee must be trained thoroughly.
Clearly define expectations: knowledge needed, performance and productivity metrics, time frames, etc.
Offer specific examples of what a successful telephone triage nurse looks like.
Create a checklist which documents the training plan/progress. Regularly share updates with the new hire.
Within the organization, broadcast the value of the telephone nurses. This keeps morale high and encourages collaboration.
Have new nurses observe experienced nurses in clinics and practice sites. This enhances their understanding of patient expectations.
Proven communication techniques, such as therapeutic rapport, must be taught and monitored. Without effective communication skills, optimal patient outcomes are impossible.
Create a weekly or daily schedule for telephone triage training. The goal of this training is to continually develop relevant skills.
Train and utilize dedicated preceptors whose primary responsibility is teaching the art and science of nurse triage. They should be proficient in the role and a recognized asset to the program.
Orientation for new telehealth nurses is most beneficial if preceptors are not included in department staffing—or in a position where they risk being called away for other duties—because the new hire might be left with nothing to do.
During training, if situations occur that require trainers to handle live phone calls, the new hire should listen and observe. Teach in real-time—then ask the new hires questions about what they've learned.
If a preceptor rotates shifts, the new hire should also rotate. Hands-on, real-time learning is the best way for new nurses to quickly develop their skills.
In my next blog, I’ll take a deeper dive into telehealth training manuals. Until then, keep telehealthing!
How Providers Can Win Big From Healthcare Consumerism Trends
What is healthcare consumerism?
Healthcare consumerism, a growing trend in the healthcare industry, is when individual patients, also known as healthcare consumers, have control over their own health affairs via digital channels.
Healthcare consumerism means patients have easy access to a wide range of healthcare services—and to a broad swath of the healthcare landscape. Points of access include websites, mobile apps, and cloud-based channels. The healthcare industry, in terms of digital service delivery, is catching up to other industries, but still lags far behind.
Consumers increasingly demand digital tools which allow them to:
Find healthcare providers who satisfy the patient's specific preferences.
Self-schedule their own appointments in health systems.
Compare hospitals and healthcare providers.
Access patient portals, where they can manage their medical services, make appointments, and learn about health policy.
Digitally order prescription drugs and request medication delivery.
Understand pricing and price transparency: out of pocket costs, financial incentives, payment plans, health savings account information, health reimbursement arrangements, flexible spending accounts data, high deductible health plans info.
Learn about healthcare provider quality and read online reviews with accurate information.
Access to Covid-19 information.
Seamless consumer access to these tools empowers patients to make the best healthcare decisions for their own health. This access also allows patients to more easily navigate the complex American healthcare system.
Because of the rise of healthcare consumerism, patients are more conscientious of healthcare costs and their associated benefits. Consumers can make value-based judgments while comparison shopping; they can choose the health insurance plan most suitable for themselves and their families. In the case of employers, the employee can help pay for and manage his or her benefits directly.
Healthcare consumerism has numerous benefits, from better care quality to lower overall costs.
Healthcare organizations that take advantage of healthcare consumerism trends can:
Improve the patient experience.
Enhance patient satisfaction.
Optimize patient care.
Strengthen patient engagement.
Drive more office visits.
The rapid development and enormous popularity of healthcare consumerism is an opportunity too ripe for health organizations to pass up.
What is the driving force behind healthcare consumerism?
Healthcare consumerism is not a new concept in the healthcare industry—but it has surged in popularity in recent years. Below is a brief history of healthcare consumerism:
Rise of value-based care, High Deductible Healthcare Plans (HDHP), and direct-to-consumer sales of drugs: In the early '80s, healthcare consumers started to participate in medical decision making with healthcare systems. In 1997, the FDA imposed stringent restrictions regarding radio advertisements for pharmaceutical products. Pharmaceutical companies began distributing more direct advertisements in their stores for medical treatments and drugs, which led to a growing consumer interest in health care.
Healthcare consumerism and digital technology: Changing consumer demands have come with the internet and smartphones. Many patients—accustomed to having instant access to almost any conceivable service on their mobile devices—now demand the same for their health affairs.
Why is healthcare consumerism important for healthcare providers?
Embracing healthcare consumerism is critical for providers who want to remain competitive in today's digital world. Healthcare consumerism allows providers to improve the health experience for consumers, who now demand full ownership of their medical services. Healthcare providers who embrace, rather than avoid, healthcare consumerism trends see numerous benefits:
Patient acquisition and patient loyalty.
Lower cost of overhead and other expenses.
A better relationship with healthcare payers.
Superior health plan opportunities.
A brand that stands out from other providers.
Greater physician satisfaction.
Exceptional service quality.
Positive patient outcomes.
How can healthcare organizations utilize healthcare consumerism trends to improve healthcare services and lower healthcare costs?
There are several ways that health systems can take advantage of healthcare consumerism trends to enhance their operations:
Online search (how to get found)
Healthcare search is local. Local search consists of two types:
Objective search: An example: Patients want to find the specialty that is the closest. This requires both an accurate address and one that is encoded in search engines. Other common objective search items include:
Types of insurance accepted.
Types of procedures performed.
Days and hours open.
Experience, age, and sex of providers.
Consumers must be able to easily find your organization by entering certain keywords on a search engine: Google, Bing, Apple, Alexa, Facebook, WebMD, Vitals, Yelp, and more. Creating and maintaining accurate and engaging profiles on these platforms is called healthcare syndication.
Healthcare syndication is a critical component of getting found in online search results. Tools like Health Desk—with its database of providers, locations, and procedures—can conduct healthcare syndication for any health practice.
Subjective search: Patients want advice—and they want to know who to trust—so that they can make the best healthcare choices for themselves and their families. You can build repute with patients by offering useful health information on your website—typically in long-form content such as blog posts. Newsletters and nurturing emails are also an excellent way for health organizations to establish themselves as thought leaders in their speciality.
Selection (how to get chosen)
Positive reviews of health practices often strengthen patient trust. 79% of consumers read reviews before making healthcare decisions.
That said, even if a provider has established trust, patients still may not schedule if the provider doesn't have an easy schedule link, or offer self-scheduling. Consumers are increasingly wary of calling health practices and waiting on hold. Providers must offer digital service suited for modern consumer demands.
Conversion (how to get the appointment)
Health organizations can optimize conversions by making it easy for patients to schedule their own appointments. Self-scheduling has countless benefits for health systems:
A satisfying and seamless consumer experience: With self-scheduling, patients aren't burdened with the need to call their provider and wait on hold. They can schedule whatever health services they need on their devices.
Lower costs: Self-scheduling takes an enormous burden off of healthcare phone staff, which means providers hire less staff and the staff they do hire need less training. This substantially reduces overhead expenses.
Physician satisfaction: A sophisticated self-scheduling platform allows doctors to utilize 100% of their schedule. Appointments are distributed evenly, are always accurate, and if a patient cancels, automatic waitlisting fills empty slots.
Scheduling optimization tools (how to fill your calendar)
Patients aren't the only ones who gain from healthcare consumerism. Physicians and support staff also see benefits—particularly in regards to scheduling. AI-powered Intelligent Scheduling automates all appointment types, from sequential to surgery, which means doctors get an accurate and equitable schedule, and support staff get fewer phone calls.
Top features of Intelligent Scheduling include:
Automatic waitlisting and rescheduling.
Round-robin scheduling.
AI-automated complex scheduling.
To learn more about Intelligent Scheduling, read our Intelligent Scheduling Whitepaper.
Post-visit scheduling and healthcare marketing (how to build on the relationship)
A holistic healthcare consumerism strategy includes patient outreach and patient engagement campaigns. These campaigns include preventive medicine information, SMS scheduling links, Covid-19 news, health education emails, and more. Combined, these marketing efforts offer a superior patient experience—which in turn drives organizational growth and expands brand visibility.
To read more about healthcare marketing campaigns, click here.
What can an employer do to promote consumerism in healthcare?
Because of the rise of healthcare consumerism, employees now demand more control over the health insurance plans offered by their employers. Which means businesses must offer flexible health insurance policies that account for individual preferences. Employers should make a wide range of health plans available—with full price transparency.
Group health plans often don't account for individual patient profiles. Each employee has unique health needs, and these needs sometimes require specific health plans. Workers often face a dilemma: they either don't need all the benefits offered by their employer's health insurance, or they need more benefits than what are offered by their employer's health insurance. In the age of healthcare consumerism, employers must make individualized care a top priority.
The future of healthcare consumerism
Almost all commerce now takes place online. Consumers order household necessities and groceries, from toilet paper to eggs, on Amazon and Instacart. Consumers book transportation and lodging, from plane flights to hotels, on Uber and Expedia. And consumers engage with health services, from scheduling to communication, on digital channels.
This digital health revolution was inevitable. It was only a matter of time before patients demanded the same control, access, and personalization from their healthcare as they got from everything else. Patients want to schedule their own appointments; patients want to compare doctors; patients want to communicate securely with their caregiver.
Modern consumers demand value-based care. They demand price transparency. They demand holistic telehealth. Healthcare organizations that offer this modern consumer experience will thrive; healthcare organizations that don’t will die.
To read more about cutting-edge patient access, check out our blog: "Uniting Patient 360 & Provider 360 Is The Future Of Patient Access."